PSA test for prostate cancer screening: should he or shouldn’t he?
Even his doctor doesn’t know for sure.
In some ways the news that the U.S. Preventive Services Task Force has stopped recommending routine prostate cancer screening through the mechanism of the PSA blood test mirrors the same group’s finding in 2009 that routine mammograms for women between 40-50 should no longer be suggested.
The problems the panel faces are very similar to those it was grappling with in the mammogram situation: a simple and relatively inexpensive screening test for a fairly common but extraordinarily nasty disease, confusing and difficult-to-evaluate statistics about whether or not the test really decreases mortality, and a treatment that has its own negatives in terms of pain and suffering (both physical and emotional). Now as then, the task force will be accused by some of cutting back on a benefit in order to save the money that would otherwise be spent to cover the test and its results. The doctors will be seen as hard-hearted and/or scientifically incompetent or simply wrong in their conclusions.
But although the two situations (mammograms and PSA tests) are somewhat similar they are not identical, with the mammogram decision actually being somewhat easier. As I wrote in November of 2009, when I disagreed somewhat with the panel’s recommendations:
The listed harms of extra mammograms seem minor although more frequent [than the harms of not doing them], the benefits admittedly less frequent but rather more major””life vs. death, for example. And deaths in the age group specified””women in their forties””involve a population of young mothers. We’re not talking about death squads for grandma here; we’re talking about mommy.
Prostate cancer is a related but somewhat different disease with even more confusing demographics and more serious (and common) side effects of treatment, presenting doctors with a host of conundrums [emphasis mine]:
Prostate cancer is the second-leading cause of cancer death among men, after lung cancer. In 2009, it was diagnosed in approximately 192,000 men. A small number of tumors are very aggressive, but the majority of prostate tumors are not likely to cause death. They grow very slowly, and only a fraction break out of the prostate, seed new tumors in other parts of the body and kill the patient. The current thinking is that about 30 percent of men in their 40s have prostate cancer, 40 percent of men in their 50s and so on, right up to 70 percent of men in their 80s. Yet only 3 percent of all men die from the disease. In other words, far more men die with prostate cancer than from it, and only a tiny fraction of prostate cancers ever cause symptoms, much less death.
But here is the tricky part: Unless there are symptoms or a finding on a physical exam, doctors generally cannot accurately predict which cancers are destined to be indolent, to sit around for years growing slowly, if at all, and those that will ultimately prove lethal.
You can see the dilemma, and it’s far worse than that facing doctors advising women about mammograms, because breast cancer—although common—is both less frequent than prostate cancer and far more reliably lethal if left untreated. What’s more, the interventions for prostate cancer are especially troubling and common in their possible side effects:
About half of men who undergo radiation or surgery [for prostate cancer] will have permanent side effects like impotence and incontinence. Up to 1 in 200 men die within 30 days from complications related to the surgery.
Those who advocate routine screening say it’s worth it in lives saved. But opponents point to studies that show no difference in mortality between the screened and the unscreened.
Until we know more, the best solution is probably (as the article concludes) to inform men of the risks and benefits of screening before they take the PSA test and let them decide whether they want to roll those iffy dice. This follows a recent trend in medicine in which patients are more and more often being asked to take responsibility for decisions that used to be the province of doctors. This is either good or bad depending on how much you want to depend on your doctor.
[NOTE: And, of course, the entire issue has insurance consequences: will PSA tests now be removed from routine coverage?]
[ADDENDUM: On a lighter note, those of a certain age may get the reference in the title and first line of this post. But for the others, here’s some help:
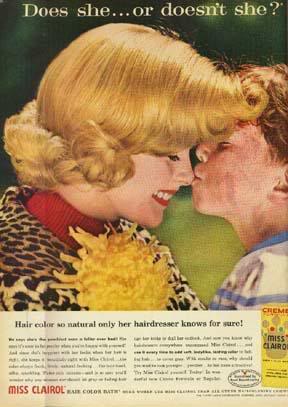
One of the most successful ad campaigns ever.]
One of the lesser-discussed points of the PSA number is that you don’t take one number in isolation. You look at trends, year after year. With a well-established baseline, it’s often a lot easier to answer the questions.
ah… the spravka is that its a social good and better
the truth is, it rations care and makes us more equal the less care we get.
this is how the old country was run, now we are much the same, but the residents dont know it, as they dont know the differnce between mercedes benz logo and the peace sign… (and believe that under communist despotism they will be more free than they ever were!)
“”Unless there are symptoms or a finding on a physical exam, doctors generally cannot accurately predict which cancers are destined to be indolent””
Which means not even your urologist knows for sure.
We spent a great deal of effort and money in the ’70s, ’80s, and 90s to discover cancer markers, among them PSA and CEA, and detection methods like mammography, on the very highly valid notion that earlier diagnosis yields higher cure rates. These fall under the umbrella of “preventative medicine”, which Hussein has assured us will lower health care costs.
The cost-control Luddites have taken charge. I guarantee that 99% of them are Democrats. I will also guarantee that every man jack of them in DC has these screens run every year, but that will never be divulged.
Screening colonoscopies will likely be next on the chopping block.
At 78, I have had PSA tests every year since age 50. Thus, I have a baseline of readings. Any sudden departure from that can be considered an indicator that something may be awry. I have been fortunate because the readings have been normal so far. However, I have friends who have had their PSA go up on them. In every case their urologists pressured them to have surgery. It was, always the old precautionary principle. “We can’t tell which tumors are aggressive so it’s best to go after all of them. And did I mention we have this remarkable new technique that gets all the prostrate with few complications.” That is how my friends have all ended up in diapers and impotent. Not one had a complication-free surgery.
As a result, I have already made the decision.
If my PSA readings do get out of the normal range, it will be watchful waiting, not surgery. My quality of living has decreased enough through normal aging, why make it worse with unneeded surgery. (The statistics are in my favor.)
Yes, I know prostate cancer that is aggressive can lead to a rather painful ending. (That’s one of the selling points for surgery.) Well, I’ll just hope that hospice can make it somewhat bearable. The statistics show that I probably have a tumor now, but it is not active yet. At my age it’s a race to see which bodily system will be the one that gives out first.
Stop getting the PSAs, JJ. Watchful waiting? Waiting for what? There is no point in spending money and getting data if one is not going to make use of the data.
“Unneeded surgery”? Who determines it was unneeded? Your pals can see the future and they all had surgery anyway?
And if by chance you should come up with prostate ca, opt for castration- it’s cheap and effective, got a guy a Nobel.
Don Carlos: about your colonoscopy statement, it’s my impression that there are huge differences. Don’t regular colonoscopies enable doctors to nip the problem in the bud, as it were (removing a cancerous or pre-cancerous polyp while still very small with no further surgery necessary and with few or no side effects)? And aren’t the consequences of untreated bowel cancer much more certain to lead to spreading disease and death?
The docs may end up limiting colonoscopies to later ages, perhaps, to save money. But I don’t see them eliminating the screenings. It wouldn’t be cost-effective, for one thing.
Pingback:neo-neocon » Blog Archive » PSA test for prostate cancer screening … | The Cancer Site
I am now ten years out from having my prostrate removed at age 57 for an aggressive cancer. All of my parts still work and yes, there are some side effects from the surgery but I will trade that any day for having the cancer. My numbers did a dramatic shift and a biopsy revealed that I had some aggressive tumors and I got several additional options and then went to work on getting the surgery done as soon as I could.
An offshoot of the follow up on my cancer which I do year after year is that my liver showed some funny stuff going on and my Dr. had a scan run on it and the liver was all right but we discovered kidney cancer which was still contained and that was then removed.
I am totally in favor of obtaining good information and then using that information to make the best decisions. When they talk about prostrate stats, they are right, if you live long enough and you are male you will probably have prostrate cancer. The next bit of information is that the older you are the slower it will grow and from what I know there is a point where due to age and the rate of change it is best to not have the surgery. As to the number of men who die after the surgery I would be interested to know how old they tend to be and what kind of health are they in before they undergo the surgery.
I don’t think any cancer indication is a one size fits all and that information and good doctors, who know the patient and like the patient, can help make the right call.
One aside is that after the surgery to remove the prostrate there is no worry about an enlarged prostrate that impedes the flow of urine, the bladder empties real fast and I am back drinking more coffee while my old timer buddies are still waiting for stuff to pass on through. I guess I am one of the happy campers because I still work full time, have a nice relationship with my lovely wife and I have not slowed down too much over the years. To me it all comes down to that fact that a life worth living is a life worth living alive since we will all be gone soon enough anyway.
Men, get the tests and follow up at regular intervals and if you find out you have a problem, be thankful because you can use the information to make your own informed decision and not have to do a hurry up and die because you found out too late.
Don Carlos, Your point about not getting PSAs is well taken. I will see if my doctor will agree to eliminate it from my annual physical. The cost is about $70 so it’s not a big financial issue. It’s normally done when routine blood tests for other health markers are done.
Watchful waiting means watching the tumor to see if it starts growing. Occasionally, the tumors do suddenly become quite aggressive, but the statistics show that most do not. If it does start growing, then one can opt for the surgery – if you are healthy enough to survive the procedure. That becomes an issue as you age. Only one of my four friends who had the surgery would opt to do it if they had the choice to make today.
It is my opinion, and I may be biased because of the sample I have personally observed, that the urologists are pushing the surgery because they really want to help and that is the big tool in their bags. Also, (this is probably way off base) it does occur that there might be a profit motive. Surgery pays far better than watchful waiting.
Opting for castration? That is essentially what happened to my friends. With total incontinence thrown into the bargain.
I had a prostate the size of a tennis ball (so it felt). So, I looked around. I started taking a beta prostate formula available off the net. It did wonders for the prostate. Pick the right one, however. I also have personal problems with being poked and prodded, etc., so I changed to a female GP. I get the blood thing done every couple years or so. I’ve had a lung removed and a brain tumor removed, so I don’t get too worried anymore. I mean, what for? I’ve still got my boyish charm, rugged good looks, and naturally curly hair.
It’s not as if some guy’s first PSA level being slightly elevated immediately leads to a surgery. As mentioned, a slightly elevated PSA may be due to several causes such as benign hypertrophy (BPH) or prostate inflammation. At worst, an MRI could be done to confirm that there are no prostate lesions.
When a baseline level has been established, any “jumps” are pretty reliable indicators that something cancerous is afoot. The levels usually rise naturally (as many men develop BPH), but that’s a more gradual rise that can be written off as such.
As far as surgery goes, it isn’t going to be performed without a biopsy of the tumor first. That biopsy will tell if the tumor is slow growing or not. There are several treatments out there aside from surgery, but any competent doctor is going to recommend one of those for a patient found to have a more aggressive pathology. They aren’t out there looking to lop the prostates out of men that will die of something else long before the prostate cancer got them.
I won’t swear to anything, I am not a doctor, a medical number cruncher, or such. From empirical evidence gathered on my own and a life lived, I would really suggest that if doctors don’t actually know then they can’t actually be sure if they are following their oath (for what oaths mean these days). Still, keeping it clean and simple, and assuming good faith, if they don’t know they have to go with ‘doing no harm’, which means not intervening.
I will not be tested. I would suggest other men not be tested if asked for advice specifically or generally. Further, I don’t think it is fair for a doctor to put a patient in the position of choosing. The doctor should minimally have a strong recommendation and perhaps a list of other doctors with whom the patient could consult. It is aboslute chicken sh*****y for a doctor to open such a can of worms then back off after doing so.
I have refreshed my memory about the issues. I went through checking all this out about three years ago when a friend who is four years younger had the radical prostatectomy. He was 71 at the time. His urologist told him that the tumor was not the aggressive type, but recommended surgery based on the precautionary principle. He regrets the decision now because his quality of life is not what he desires.
Here’s a site to check out for all the men who might be wondering what the options are and what the odds are of successful treatment:
http://tinyurl.com/3upxycg
A quick glance at the charts will show that when the patient is diagnosed with prostate cancer younger than 70, surgery seems to be the gold standard. Older than 70, radiation seems better suited and beyond 80 watchful waiting is the best course. All have their advantages and disadvantages. I’m glad this has come up because it has forced me to revisit the issues and reinforces my thinking.
Obviously my friends have been unlucky because the charts show that only 20% have incontinence and impotence as a result of the surgery. Pick your surgeon carefully!
All the chatter is about prostate surgery. Why? Radiation therapy is equally effective.
Neo: No early cancer detection method is based on cost-effectiveness. There is no free lunch.
Colonoscopy is not “cost-effective”. Surveillance colonoscopy cost Medicare about the same as ALL radiation therapy when last I looked (some yrs ago).
“Preventative” care costs every time, and in terms of detecting things like diabetes and hypertension early, there is No Cure. Zip. Nada. So, aside from detection costs, there are all the costs of earlier treatment, and it is by no means clear that this yields cost savings 30-40yrs down the road. What it does is save and extend lives-no small thing- but assigning a value to one year of life is a fool’s or an elitist’s exercise.
Life ain’t free!
JJ, one PSA at $70 x 5 million tests/yr= $350 million, just for example. Probably more than 5 million PSAs are run each year, BTW. Medicare don’t like that. Neither do I, if you will not use it in your decision-making when it rises, which it will.
“Dooms” remarks are not worthy of comment.
My father died of prostate cancer. It took a few years to kill him but it ended painfully and badly. I’m now close to the age he was when he was diagnosed. I get my PSA checked annually and it has been normal. If I get a bad reading, I’ll opt for the treatment that Andy Grove (of Intel fame) chose. He’s still going strong.
Pat Dooley,
Thank you for making Andy Grove’s paper available. It sure covers the bases and in a very intelligent manner. Not many men would do this kind of research. I know I wouldn’t. I have added it to my favorites and intend to share it with many of my friends – the ones who haven’t had a diagnosis yet.
Since I am Puget Sound it is nice to know that the radiation expert is here. I hope he or some of his associates are still around.
Don Carlos,
For one thing, you are wrong about diabetes being incurable. Why or how, I am not sure. But having blood sugar levels beyond the range of my meter about four years ago, my A1C has been well below 6.0 for the last year.
Beyond that, I don’t think you or I read the story right. If a very small percentage of those die from the cancer, even a smaller number compared to those who receive treatment, than you are clearly off your head (or I misread). Too late tonight to check, but that is what I gathered from my initial readings.
If I am correct that you have spoken correctly about “not worthy of comment”, but have mistaken the target.
Don Carlos: there’s quite a bit of research indicating that colonoscopies are cost-effective, depending on the schedule (see this, for example). That’s not to say that a personal decision as to whether or not to have a colonoscopy should necessarily be based on cost-effectiveness. But decisions on whether Medicare, etc., should cover them often are, I believe.
Love the Clairol ad. Reminds me of when I was a kid and my mom would give the house a good cleaning and lay out her Ladies Home Journals and McCalls and other Womens magazines before the other mothers of the Womens Club would visit. They would have coffee and home baked cakes and pies and cookies of different kinds and ooo and ahh over the magazines. As a young boy watching them I thought there must be something very special perhaps magical about those magazines and after they’d gone I would sneek a peek and one of the things I remember is the Clairol ads and how then these magazines celebrated mothers and family. So here I am an older gentleman reading about the PSA test and whether it’s any use in detecting prostrate cancer and when I go outside I’m surrounded by tattooed weenees, socialist jerks and people that hate America and on TV they celebrate 16 and Pregnant and Chaz Bono. Then I see this ad and all I can think of is how much I miss the 50’s. Thanks for the memories Neo.
Don Carlos,
Up until this year Medicare did not pay for the annual physical. I paid out of pocket. With the doctor’s time and blood tests I think it ran about $300, total. Suddenly, this year Medicare is paying for the physicals. It does not compute when Medicare is running out of money. But then not much the bureaucracy does makes all that much sense.
Neo-
Your link compares the cost-effectiveness of two different kinds of surveillance colonoscopy schedules. That is not the same as showing the procedure itself, regardless of schedule, is cost-effective per one life “saved”. Cost-effectiveness always compares the cost of A to the cost of B.
My point remains one cannot assert that cost X expended to save Y lives is cost-effective without ascribing a value (and thus a cost) to a year of life saved (or lost), or a life saved (or lost).
Hey guys-
Grove’s story is a rather old and now outdated one. Things do change over time. His was before robotic surgery and the now widely available IMRT radiation therapy, for example.
Medicare reimbursement has a lot to do with what’s available vs. what’s recommended. Para exemplar, as reimbursement for prostatectomies has fallen, many urologists have decided it ain’t worth doing anymore. In many larger communities, urologists have banded together in ownership of a radiation oncology facility, which has a rad onc MD to whom they refer, and all those prostates get IMRT therapy, which requires expensive equipment and is thus better reimbursed. Now the urols get a share of the technical reimbursement and thus earn without operating.
The rad oncs that own their own equipment, and hospitals with rad onc depts, are powerless. But the urols still refer to those two, principally the poorly insured and Medicaid patients.
Don Carlos: so are you saying that the article I link to in the post that discusses all the negatives of surgery is outdated because surgery is rarely used any more? If so, why does the article (and the recommendations of the panel) discuss surgery so prominently?
Are you also saying that the urologists recommending radiation rather than surgery do so because it satisfies their own needs (more money and less work)?
By the way, these are real questions of mine, not rhetorical ones. You have a lot more expertise in this field than I.
Neo-
The link I went to was on cost-effectiveness with colonoscopic surveillance. Not the one on prostate.
As to prostate, the cure outcomes are basically the same, method v. method v. method of treatment. It is the adverse effects that differ, and the time involved (implant recovery is short, surgery more arduous and longer, IMRT radiation takes 8 weeks).
Re your 2nd query: you have it exactly correct-more (or same) money, no operations, less med mal concern for the urologists.
Don Carlos: from the small amount I’ve read about surgery vs. radiation for prostate cancer, my impression is that radiation is even more likely to cause impotence (permanent as opposed to temporary?) and surgery more likely to cause incontinence. But the figures are hard to get. Do you happen to know them?
It’s all about playing the odds, but as to one person, it is always a single coin toss.
The impotence #s change as the technologies change. Both can do it, but as to surgery, it is operator-dependent, since it involves the sparing of small nerves. Not so with radiation- the nerves always get the dose. A urologist who only does one prostate a week will have a much higher rate of impotence than one who does 2-3 cases a day. The mechanism of impotence post radiation remains basically speculative-neurologic or microvascular injury or both? One does not have tissue to examine after radiation! But there is Viagra.
Patient selection is a major factor. Resected patients are on average younger, and thus more likely to retain potency. To play on a Viagra commercial, “If you’re not heathy enough for sex, you are not healthy enough for a prostatectomy.”
Bottom line: I do not want to cite a figure of one vs, the other, since they are not “pure” #s, fixed in time.
Yes, surgery causes incontinence (again, operator-dependent) and radiation does not. But competent surgery basically does not pose a risk of serious, delayed-onset, chronic and unremitting rectal injury (diarrhea, urgency, bleeding, pain), whereas radiation does; small, but not zero.
Thus goeth the surgery v. radiation controvery, as it has for decades. Outcomes (low, flatline PSA graphs over time) essentially identical, pain and time of treatment and risks different. So decisions are now made in significant part by those and economic factors.
Artfldgr has it right. This is about letting the proles die because it’s cheaper then treating us. The Inner Party members will get their screening and treatments. Us? We get a hospice bed and morphine. You think that the higher cancer death rates for the Euroweenies is a accident?
It’s a feature, not a bug.
BJB-
Slick fellers, them Elites. They actually got the Euroweenies to buy it; they still do. Been happening here for the past 20-some yrs. Creeping incrementalism, sowing just enough seeds of doubt, keeping the ignorant ignorant, and then when the moment is right, BLAM, and we’ve got Obamacare.
Staying power is what they’ve got, and we do not.
I gotta take my hat off to ol’ Gramsci. He read us right.
On the subject of cancer generally, may I recommend “The Emperor of Maladies”? I just finished it – it was as gripping as a thriller, and I’m not normally a big non-fiction reader.
Gentlemen, I have learned a lot from listening to you here. My husband is 44 and has just started getting PSA tests during his “executive physicals” (which he hates but which are required in his position). One of his high school friends was among the people who worked on the development of the PSA test, so it’s never occurred to the hubby to question whether to GET the test; I’ll be talking with both the hubby and the friend about it, now that I’m better informed.
After all the decades of avoiding the European disease that most of our ancestors fled from we now have the same double digit unemployment, crippled stagnant economy and a deeply entrenched bureaucracy that is essentially in business for itself.
And even know when the whole European experiment is collapsing we still have people who think it’s the best thing since sliced bread.
And all you have to do is convince someone that he other guys stuff should be theirs and then promise to take it away from that other guy and give it to them.
And interesting conversations like the one here about treatment choices? They don’t have them. The proles get what their given and die when they’re supposed to.
What’s not to like?
What could go wrong?
“For one thing, you are wrong about diabetes being incurable. ”
AFAIK it’s incurable but often misdiagnosed (iow elevated blood sugar levels and/or swinging insulin levels are automatically diagnosed as diabetes even if they are not always diabetes by far), and if something else (or “proto-diabetes”, iow the symptoms could become diabetes but haven’t yet) it can be handled and they disappear.
It’s so simple nowadays for doctors to make a life changing diagnosis that will put you up for a lifetime of expensive doctor’s visits and medication, a highly lucrative prospect for them.
So they may well never look beyond those diagnoses (and what’s less lucrative for a doctor than to get someone diagnosed with diabetes, he’ll have to be back several times a month for life to buy more insulin and test strips?).
Not saying it’s (always) malice, but it’s also an easy way out.
With governments constantly putting out scare stories about “diabetes epidemic”, “cancer epidemic”, “obesity epidemic”, etc. etc. patients expect to have all that, to see it diagnosed (and I’d not be surprised if they’re pushed to diagnose it by regulators as well as by drug companies offering nice incentives and kickbacks for drugs sold, which they do) is almost a relief.
“Surveillance colonoscopy cost Medicare about the same as ALL radiation therapy when last I looked (some yrs ago).”
Maybe. But per patient? If there’s a million colonoscopies performed each year and 10.000 radiation therapies (e.g.), radiation therapy can per patient cost 100 times as much as a colonoscopy and still not be more expensive as a total figure in Medicare’s annual reports.
““Preventative” care costs every time, and in terms of detecting things like diabetes and hypertension early, there is No Cure. ”
If caught early (in “proto” stages, so to speak) these can often be kicked in the nuts before turning into the full blown (and indeed incurable) condition, improving lives and saving cost in the long run. See above as to why this isn’t done more often.
One thing I did not see mentioned in the above comments is a new method of treatment for both prostate and breast cancer called Proton Therapy. It had only been available at one hospital for several years but now there are nine, I believe, Proton centers throughout the country with more under construction. If you are facing cancer take a moment to research the benefits offered.
JTW-
I fear you misunderestimate the point I tried to make:
Surveillance colonoscopy is preventative. It is for detection.
Radiation therapy is used on people that have cancer. It is not for detection, it is actual treatment.
As to the profit motive by MDs, please be aware that diabetics do not get insulin/test strips from MDs, but from pharmacies. Docs in increasing #s are refusing to see MCare and MAid patients because it flat ain’t worth their time: it is not that they do not earn enough from them; they lose money. It costs them more to see these patients than they are paid.
Sorry for having to explain the obvious.
Don Carlos: another question—I know that a surveillance colonoscopy is for detection, but if a cancerous or pre-cancerous polyp is detected in the same procedure is not the polyp removed, which would be (in a way, anyway) a form of treatment? When does prevention become treatment, especially if no further treatment in the form of radiation and/or chemo is necessary? I have read that if a polyp is removed it only adds about $200 or maybe $300 or so to the cost of the procedure.
So, wouldn’t colonoscopies be considered treatment sometimes (in some percentage of cases; I don’t know how often such polyps are found), and wouldn’t that have to be compared to the cost of treatment of the same cancer at a much later date (that is, the cost of chemo and/or radiation and/or a big surgery and/or ostomy care if necessary, and/or death?)
By the way, I found this study and this finding:
Neo :
May I be so bold as to say you’re thinking like an attorney?
All small polyps are not premalignant, and only a modest % of the pathologically “atypical” polyps are destined to become cancer if left alone. But all polyps are removed at colonoscopy, for pathological examination (which is a cost above colonoscopy itself), for reasons of medmal defense, and for reason of correct care. So whether it’s prevention or treatment, well?
A cancerous polyp is not a polyp; it is a cancer, possibly not yet invasive, but still a cancer.
I did not read your link because my computer is having fits of lethargy. But the cost per yr of life saved kinda depends on the reimbursement method (MCare vs Non-MCare) and it kinda depends on what a year of life is worth, e.g. at 60, vs 70. Cost per yr life saved is a convenient but curious metric. One person does not gain a year, or X years, by having colon cancer prevented. I am not intellectually or emotionally equipped to speak to that, and never have been. A life is a life, in my book. I don’t manage populations; that is a task for the unfeeling, like Sibelius.
Dunno if this answers you in any way!
Don Carlos: I wasn’t really trying to make any point, just curious about whether polyp removal is considered prevention or treatment when it’s classified for the purposes of research.
I agree that it’s a terrible conundrum to try to measure lives in dollars, and somewhat offensive (at least to me), but when we’re talking about reimbursement for procedures (especially when it’s government programs making the decision about whether or not to fund a medical intervention), it seems to become inevitable.
I also think that there are a lot more unknowns in medicine than most people suppose. For example, it’s probably unknown what percentage of suspicious polyps would go on to become cancerous if left alone—or is it?
Polyp removal in ‘normal’ patients (excluding those with, for example, familial multiple polyposis) is considered preventive.
The risk of a small (<1cm) polyp becoming a malignancy if left alone, over time, is about three-fold greater than the risk of developing colon cancer without a prior polyp. So if a clean colon has a 1:1000 chance of a cancer, the risk with a small polyp becomes 3:1000, just to show the relative difference (these numbers are illustrative, not based on actual incidence).
There are about 100,000 new cases of colon, plus 40,000 rectal, cancers per year in the US. The incidence has declined by 2-3% per year over the past 15-20 years. Due at least in part to plucking out lots of small polyps at lots and lots of colonoscopies!